 Got a camper in your house with HBV? Are you concerned about filling out the mountain of paperwork associated with sending your child off to a day camp, or over-night camp this summer? The paper work is not consistent from camp to camp, and quite often probing health questions may be asked. If you’re a parent with a child with HBV, seeing it in print will likely be unnerving.
Got a camper in your house with HBV? Are you concerned about filling out the mountain of paperwork associated with sending your child off to a day camp, or over-night camp this summer? The paper work is not consistent from camp to camp, and quite often probing health questions may be asked. If you’re a parent with a child with HBV, seeing it in print will likely be unnerving.
Camp forms will have a health history section which may start with the following:
Does the camper have a history of any of the following? Check all that apply.
A long list of conditions including things like asthma, diabetes, migraines, surgery, and physical disabilities may be on the list, along with the possibility of “other” accompanied by a blank-line. It is also possible there will be a box specifically for hepatitis B.
Personally, I would NOT check the “other” box, nor would I list hepatitis B on the line following “other”. I would also NOT check the box if the medical history specifically refers to hepatitis B, or viral hepatitis. I would also not consider my child’s liver biopsy as a “surgery”. There is NO need to offer up unnecessary information that does not pertain to the safety of your child’s camp experience.
Here is my thinking. A condition like diabetes, asthma, or even allergies may well require acute care while the camper is at camp. A nurse or staff person may be responsible for administering medication for this acute condition. Children with hepatitis B are rarely symptomatic and have compensated livers. They can take prescribed or OTC drugs you and your doctor have noted on the paperwork. The likelihood of an emergency occurring due to the child’s HBV is nil, and in the event of an unrelated emergency, your child’s liver would tolerate emergency services necessary to stabilize him. Life saving decisions would be left in the hands of an emergency care facility and ER trained staff.
There is always the concern that camp staff should be notified in order to protect them in case of accidental exposure, but I believe this is unnecessary. We live in a small world and disclosing a child’s HBV status to camp staff may come back to haunt you. HBV is vaccine preventable, and staff should be up-to-date on their immunizations. Standard precautions training is a must for camp staff. This will protect staff and all children from potential exposure to body fluids, such as blood, if protocols are properly followed.
Because HBV and HCV are typically asymptomatic, and children are not screened prior to attending camp, you have to assume that someone else at camp will have HBV, HCV or even HIV.
If you can’t get past concerns regarding your child and her HBV, then perhaps you need to re-consider camp for this summer. We all have our own comfort level, and we get there in our own time. However, my advice is to relax, fill out the forms, and send your happy camper off to camp!










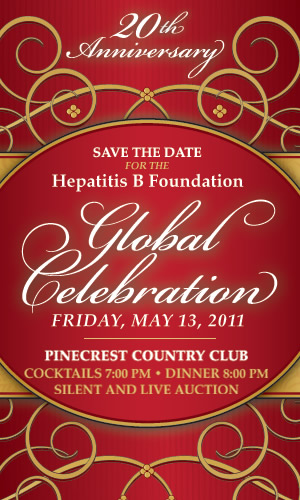 The Hepatitis B Foundation
The Hepatitis B Foundation 



