The American Gastroenterological Association (AGA) has released updated guidelines to prevent and treat hepatitis B reactivation (HBVr) among at risk populations. Hepatitis B Reactivation is a serious health issue for many people undergoing treatment for cancer or people on other medications. Learn more about HBVr here.
Immunosuppressive medications are used to treat many different health conditions and most types of cancers. Sometimes, these medications can cause sudden increases in HBV DNA levels and cause reactivation. This can lead to liver failure, severe liver damage and death. Because reactivation can happen to anyone, it is important to test for hepatitis B before starting any kind of immunosuppressive treatment as this can help doctors understand the patient’s previous or current exposure to hepatitis B and prevent reactivation altogether (Ali et al., 2025). If someone is at risk for reactivation, it can be prevented, and this testing helps to ensure that.
The new guidelines have identified individuals that are most at risk of HBVr according to their hepatitis B status and the immunosuppressive medications they are receiving.
People who are positive for chronic hepatitis B are at the highest risk if they take the following medications
- Anthracycline derivatives, anti-tumor necrosis factor (TNF) agents, or anti-interleukin-6 (IL-6) therapies.
- B cell-depleting agents (E.g., rituximab), chimeric antigen receptor (CAR)-T cell therapies, or cytokine/integrin inhibitors.
- Tyrosine kinase inhibitor (TKI) therapies or Janus kinase (JAK) inhibitors.
- Liver cancer treatment -transarterial chemoembolization (TACE))
- Co-infected with hepatitis C and on direct-acting antiviral (DAA) therapy.
- High doses of corticosteroids for longer than a month
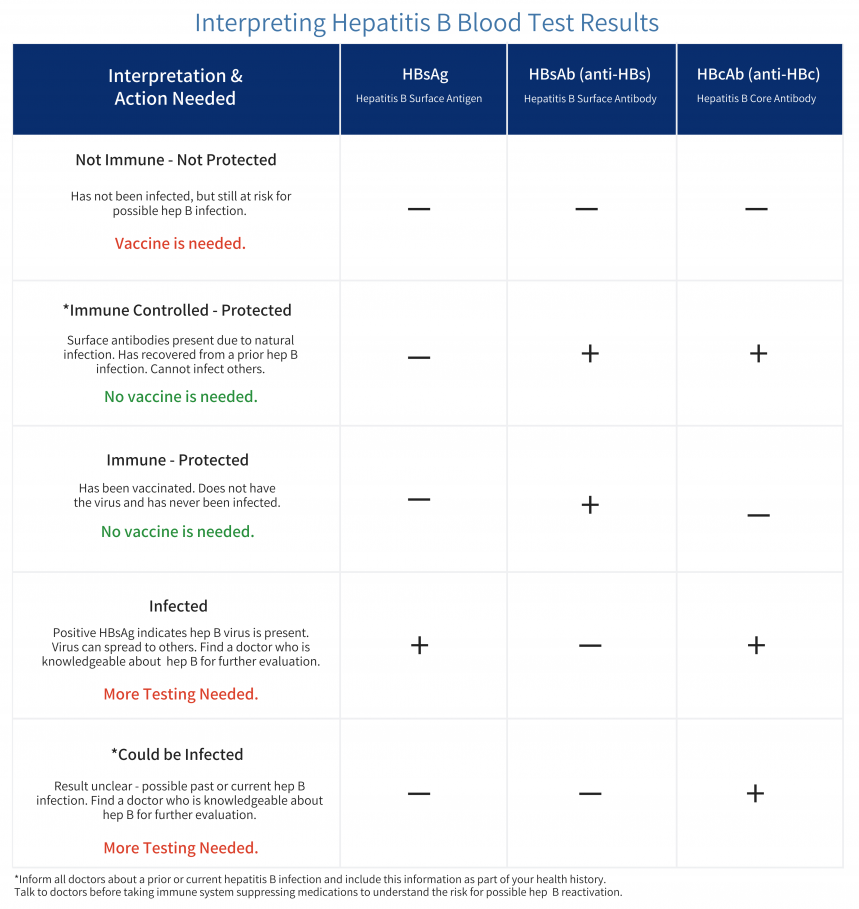
People who were previously exposed to hepatitis B (through a positive anti-HBc) or if they tested negative for surface antigen are at the highest risk if they take rituximab (a cancer treatment drug) but are at a moderate risk if they take any of the above-mentioned medications or treatments (Ali et al., 2025).
HBVr can progress rapidly, which is why screening for hepatitis B, prior to beginning treatment for cancers is important. If you take any of the mentioned medications, it is best to discuss with your doctor about your risk of reactivation. If you know about your hepatitis B status, you should disclose it to your provider or ask to get tested for hepatitis B to learn about your risk of reactivation. In the United States, all adults over 18 years of age are recommended to get tested for hepatitis B at least once in their lifetime.
- Learn more about the updated guidelines here.
- Learn more about hepatitis B Reactivation on our B Heppy Podcast here.
References
Ali, F. S., Nguyen, M. H., Hernaez, R., Huang, D. Q., Wilder, J., Piscoya, A., Simon, T. G., & Falck-Ytter, Y. (2025). AGA Clinical Practice Guideline on the Prevention and Treatment of Hepatitis B Virus Reactivation in At-Risk Individuals. Gastroenterology, 168(2), 267–284. https://doi.org/10.1053/j.gastro.2024.11.008