At the Hepatitis B Foundation, we have many research and programs throughout the year. With the Association of Asian Pacific Community Health Organizations (AAPCHO), we co-founded and co-chair Hep B United, a national coalition dedicated to reducing the health disparities associated with hepatitis B by increasing awareness, screening, vaccination, and linkage to care for high-risk communities across the United States. The coalition works to reduce the impact of hepatitis B through prevention and education efforts, addressing perinatal transmission, improving screening and linkage to care, contributing to national surveillance data, and advocating on a national level.
Last year, the Hepatitis B Foundation offered mini-grants for one year to Hep B United coalition partners working on hepatitis B education, screening and linkage to care activities. These grants ranged between $5,000 to $10,000 each. The mini-grants were offered to enhance the capacity of Hep B United coalition partners to conduct HBV education, testing and linkage to care in their local Asian American, Native Hawaiian and Pacific Islander (AA & NHPI) communities to advance the hepatitis B priority areas of the U.S. Department of Health and Human Services’ National Viral Hepatitis Action Plan (VHAP).
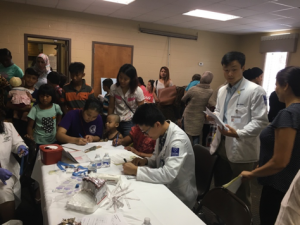
The 2016-17 project year offered grants to 9 coalition partners, which included Center for Pan Asian Community Services, Inc (CPACS), Hepatitis B Initiative-Minnesota (HBI-MN), Midwest Asian Health Association (MAHA), Hepatitis B Initiative-DC (HBI-DC), Asian Services in Action (ASIA), Asian American Community Services (AACS), Asian Pacific Health Foundation (APHF), and HOPE Clinic. Together, Hep B United coalition partners screened 4,649 people, educated and reached out to 11,884 people, and distributed 13,112 handouts. Some coalition partners were featured in newspapers, on TV with 496,189 views, and in a social media video. Mini-grantees also participated in activities such as developing key partnerships in local communities, providing linkage to care, and conducting provider training. One coalition partner also screened the “Be About It” documentary.
For 2017-2018 mini-grants, six Hep B United coalition partners (listed below) were recently awarded mini-grants. We are excited to kick off these projects and look forward to their future endeavors and results.
· Asian American Community Services (Columbus, OH) -AACS’ Live Healthy – Hep Free project will use the H+EAL model to increase HBV education and awareness and encourage testing by targeting high school students and their parents.
· Asian Pacific Community in Action (Phoenix, AZ) – APCA will be organizing community town hall events in collaboration with the #justB campaign across Maricopa County to collect and share stories that promote increased awareness and proactive approaches to treatment for hepatitis B.
· Asian Pacific Health Foundation (San Diego, CA) – APHF will be working to increase community knowledge and awareness of hepatitis B, determine gaps in knowledge, develop in-language education materials, and provide hepatitis B screening within high-risk communities throughout San Diego.
· Asian Services in Action (Cleveland, OH) – ASIA will be using community health outreach workers to increase HBV education and screening, including outreach to AAPI businesses in Akron and Cleveland, OH.
· Center for Pan Asian Community Services (Atlanta, GA) – CPACS’ project focuses on expanding their Atlanta-based hepatitis B coalition, increasing the number of Georgia AAPI community members who know their HBV status through community and provider education, and improving testing and linkage to care services throughout the city.
· Philadelphia Department of Public Health (Philadelphia, PA) -The Perinatal Hepatitis B Prevention Program auxiliary project will create new education modules for prenatal and pediatric care and conduct on-site provider education sessions to improve knowledge and care for infected mothers.
The 2017-18 project period expanded its priorities to address perinatal transmission and education through storytelling efforts with the #JustB Storytelling Campaign in addition to screenings and linkage to care. The overall success of the Hep B United mini-grants has been proven through the significant number of high-risk populations educated, screened and linked into appropriate care for hepatitis B. We look forward to updating you further in the coming months as we continue to highlight the national work of the Hepatitis B Foundation and Hep B United partners around the U.S.



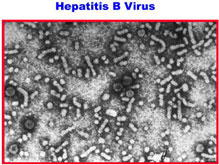
 How many years have you had hepatitis B? The longer you’re infected, the higher your risk of liver cancer.
How many years have you had hepatitis B? The longer you’re infected, the higher your risk of liver cancer.





 The
The