Please welcome guest blogger, Ram Meyyappan, senior editor of Social Security Disability Help as he provides advice on applying for Social Security Disability Insurance or Supplemental Security Income should your HBV prevent you from working.
Please welcome guest blogger, Ram Meyyappan, senior editor of Social Security Disability Help as he provides advice on applying for Social Security Disability Insurance or Supplemental Security Income should your HBV prevent you from working.
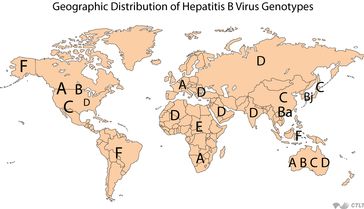
Hepatitis B (HBV) is often referred to as a “silent infection” because those chronically infected may have few or no symptoms, or may not be unaware of their infection for decades. However, over time, the risk of serious liver disease is certainly possible and symptoms can range from mild to severe. Severe symptoms rarely occur with an acute HBV infection, but can have very serious outcomes. If your condition is severe to the point that you can no longer continue to work, you may qualify for SSDI (Social Security Disability Insurance) or Supplemental Security Income (SSI) benefits from the Social Security Administration (SSA).
You can learn more about SSDI and SSI here
Hepatitis B and Qualifying for Benefits
When you submit an application for Social Security Disability benefits an adjudicator will review your file and compare your condition with a listing of conditions known as the SSA Blue Book (http://www.ssa.gov/disability/professionals/bluebook/). This Blue Book contains a listing of conditions and qualifying criteria that may qualify an individual for Social Security Disability benefits. Unfortunately Hepatitis B does not have its own listing in the Blue Book. You may still be able to qualify for disability benefits, however, if you are able to prove that you suffer from an associated condition (such as depression) that is included in the Blue Book. Some of the conditions that may qualify an individual for Social Security Disability benefits that are listed in the Blue Book and that may be associated with Hepatitis B include:
- 5.05 Chronic liver disease
- 5.08 Unexplained weight loss
- 5.09 Liver transplant
- 12.04 Affective disorders
If you are applying for disability benefits based on an associated condition that is listed in the Blue Book, you must provide medical documentation proving that your condition is severe enough to meet the criteria of that specific listing. For example, in the case of chronic liver disease, you must be able to prove that:
- You are hemorrhaging from esophageal, gastric, or ectopic varices or from portal hypertensive gastropathy and it has resulted in hemodynamic instability and required hospitalization for transfusion of at least 2 units of blood; or
- You suffer from ascites or hydrothorax that is not attributable to other causes, despite continuing treatment, as prescribed, and that the condition was present during at least 2 evaluations that were at least 60 days apart within a consecutive 6-month period; or
- You suffer from spontaneous bacterial peritonitis with peritoneal fluid containing an absolute neutrophil count of at least 250 cells/mm3; or
- You are suffering from end-stage liver disease with SSA CLD scores of 22 or greater.
If you are not suffering from a condition that is listed in the SSA’s Blue Book, you may still be able to qualify for disability benefits under what is known as a vocation allowance. In order to do this, however, you will have to prove that you are unable to perform any type of work activity whatsoever. This can be done through medical findings, laboratory reports and a residual functional capacity form. In the case of Hepatitis B, your condition must be very advanced and severe in order to qualify. Unless you are suffering from end-stage liver disease, you may have a hard time qualifying for benefits based on this condition.
Applying for Social Security Disability Benefits with Hepatitis B
To apply for Social Security Disability benefits, you can apply online at the SSA’s website (http://www.socialsecurity.gov/pgm/disability.htm) or apply in person at your local Social Security office. You will want to make sure that you have all of your medical evidence ready when you go to submit your application for benefits.
It can be very hard to prove that you qualify for Social Security Disability benefits when you are applying based on a condition that is not included in the SSA’s Blue Book. Because of this, you may want to consider retaining the services of a disability attorney prior to submitting your application. A disability lawyer can help you gather the evidence that you will need to prove your case. These attorneys will know which condition, if any, may qualify you under the SSA’s Blue Book or how to prove that you qualify based on a vocational allowance.
Article written by Ram Meyyappan, senior editor of Social Security Disability Help. Please refer to the Social Security Disability Benefits Help website for additional information. (www.disability-benefits-help.org)


![5-17-13[1]](https://wp.hepb.org/wp-content/uploads/2013/05/5-17-1311-1024x701.jpg)