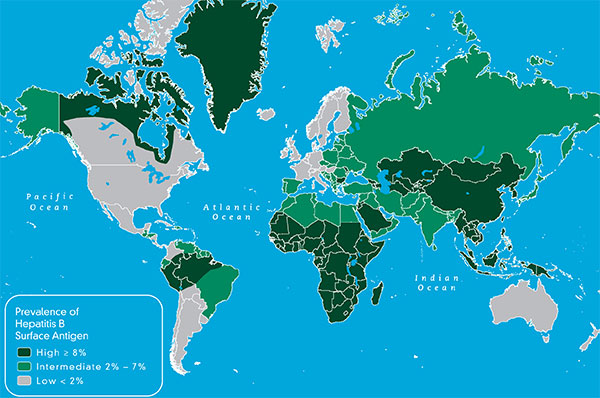
 Do you know the stage or phase of your chronic hepatitis B infection? Quite often people may refer to themselves as “hepatitis B carriers”. This statement by itself does not say anything about your chronic hepatitis B infection except that you are someone who tests positive for hepatitis B, and that you are HBsAg positive.
Do you know the stage or phase of your chronic hepatitis B infection? Quite often people may refer to themselves as “hepatitis B carriers”. This statement by itself does not say anything about your chronic hepatitis B infection except that you are someone who tests positive for hepatitis B, and that you are HBsAg positive.
The names of the stages or phases of HBV may vary with the liver society or over the years, but they reflect the natural history of the virus. It can be helpful for your doctor to determine if you are in the immune tolerant, immune active or clearance phase, the inactive carrier phase, have developed HBe negative chronic hepatitis B, or if you are in an HBsAg negative phase. It may take a few months or even half a year to accurately determine the phase, and then your doctor can talk to you about possible treatment options and whether or not treatment would benefit you at this time. Remember, hepatitis B is typically not an emergency, so try to relax with the process knowing you may not have immediate answers.
If you are acutely infected, you also follow the natural course of the virus in a matter of months (clearance of an acute HBV infection within 6 months is considered an acute hepatitis B infection). However, at the end of 6 months, those acutely infected will have a resolved infection, and will no longer be HBsAg+. If you are chronically infected, you will pass through many of these phases too, but unfortunately you will likely never get to an HBsAg negative or resolved phase. The journey from phase to phase is different for each person and the time it takes to move through these phases varies along with the amount of liver damage that occurs.
The importance of a good liver specialist or knowledgeable doctor cannot be over emphasized. These stages and phases may seem simple to understand, but not everything is black and white. There are often “gray areas” between phases or time between phases where bloodwork and other diagnostic data must be carefully monitored. Results vary with the patient. New evidence indicates there may be more damage occurring during this gray area than originally thought. There may be a missed opportunity for treatment during this time.
The importance of being actively involved in your hepatitis B care can not be overstated. Tracking your lab data over time and putting it into an excel spreadsheet or graphing the data may help you understand what is happening with the virus and may even be helpful for your doctor, so don’t forget to request copies of all lab results. You are more in control than you think. Get involved with your care!
Once you have confirmed that you have chronic hep B, you need further testing to determine your HBeAg status. Those with chronic hepatitis B are either HBeAg positive or negative. If you are HBeAg positive, you have a higher hepatitis B viral load/HBV DNA and are more infectious to others. People who are HBeAg positive are either in the immune tolerant stage or the immune clearance stage or in a gray zone. Repeated labs over time will help clarify this for your doctor.
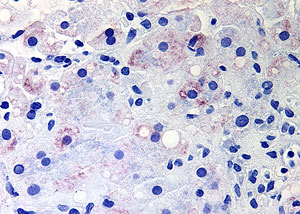
If you are in the immune tolerant stage, you are HBeAg positive and have a high viral load. You will have normal or very mildly elevated ALT (SGPT) levels and mild or no inflammation or damage to the liver. This is very common with chronically infected young children who may have viral loads in the millions or even billions. During this time the virus is actively replicating in the liver, but the immune system has not recognized the virus so it is not trying to kill the infected liver cells. It is not the replication of the virus that kills liver cells, causing liver damage, but it is the response of your immune system to these infected liver cells.
During the immune tolerant phase the virus is happily replicating, completely unchecked by the immune system, which accounts for the high viral load and lack of liver damage during this time. People in the immune tolerant phase may remain in this phase for a couple of years, or it may be decades. Treatment is not typically recommended during this phase. However, for those that have been in this phase for decades, treatment is something likely recommended by a liver specialist. There is also the concern that a person may be in a gray zone where ALT elevations and subsequent liver damage may be occurring but may be missed. This emphasizes the need for very careful monitoring by a knowledgeable doctor and the possible discussion for treatment.
What happens when you move into the HBeAg-positive chronic hepatitis /Immune Reactive / Immune clearance phase? Read more.