In 2013, an integral ruling by the United States Department of Justice (DOJ) took a major step towards ending one of the many forms of discrimination that hepatitis B patients face. The settlement made it illegal for medical schools to discriminate against students due to their hepatitis B status. Six years later, the words of

Thomas E. Perez, former Assistant Attorney General for the Civil Rights Division, still ring true: “Excluding people with disabilities from higher education based on unfounded fears or incorrect scientific information is unacceptable”. Unfortunately, many medical schools – both nationally and internationally – fail to acknowledge this.
Since the court settlement in 2013, we’ve received an increasing number of patient complaints regarding medical school discrimination. Some students completed all of their classes only to be told that they couldn’t participate in their clinical experience (which is a degree requirement) due to their hepatitis B status. Other students have had their acceptance to a school revoked because they tested positive for the infection. Both situations are considered illegal under the Americans with Disabilities Act (ADA).
What You Should Know:
- You are protected by the law: Under Titles II and III of the ADA, it is illegal for entities, including schools, to discriminate against students based upon a disability like a chronic illness. In addition, institutions are required to make arrangements, policies, and procedures when needed in order to ensure that those titles are being followed.
- You are not a threat: It is important to note
 that discriminatory policies are often outdated and should be unnecessary – in both schools and the healthcare field – as long as the appropriate procedures and precautions are followed.
that discriminatory policies are often outdated and should be unnecessary – in both schools and the healthcare field – as long as the appropriate procedures and precautions are followed. - The Centers for Disease Control and Prevention (CDC) Recommendations are in your favor: In 2012, the CDC worked with us and a few other organizations to update their recommendations for managing healthcare students and workers with hepatitis B. Amongst those changes were no requirement of telling patients of a health-care provider’s or student’s hepatitis B status, using HBV DNA instead of hepatitis B e-antigen status to monitor infectivity; and, for those requiring oversight, a threshold value of HBV DNA considered “safe” (<1,000 IU/ml). They also state that “for most chronically infected providers and students who conform to current standards for infection control, hepatitis B infection status alone does not require any curtailing of their practices or supervised learning experiences. “
What Discrimination Looks Like:
Sometimes, schools’ discriminatory actions are obvious but oftentimes they are not. Despite direction from the DOJ and requirements in the specified in the ADA, some institutions have not created standardized arrangements or policies for people who have hepatitis B. Other schools are not aware that turning away certain students based on a disability is illegal.
Discriminatory policies by schools may include:
- Asking students to show proof of hepatitis B surface antibodies (HBsAb)
- Revoking acceptance to the school based upon positive hepatitis B status (HbsAg)
- Requiring undetectable viral load or e-antigen negativity for completion of clinical rotations
As an example of a discriminatory policy, Lehigh Carbon Community College states that: “The health care agencies for clinical experiences have specific health requirements that must be met by each student. The program requires proof of personal health insurance during enrollment in the nursing program. Admission to the program may be revoked upon review of these results. (1) Positive Hepatitis B Surface Antigen (2) Titer Levels for Hep B antibody level.”
This policy does not comply with the CDC’s current recommendations and seems to be a violation of the protections afforded by the ADA. You can view this policy on page 15 of their student handbook.
A good, non-discriminatory policy should be transparent and specific. One example of this is Rutgers University. The policy is in line with, and clearly references, the CDC’s most recent guidelines and provides a clear path on how to proceed based upon each student’s infections:
“Individuals who are found to be infected with HBV shall be counseled by the Student Health Service director or Occupational Medicine/Employee Health Service director in accordance with current guidelines from the CDC.”
You can view these guidelines under section H, category 40.3.5 of their policy website.
What To Do If You Face Discrimination:
If you believe that a school is discriminating against you based on your hepatitis B status, there are a few important steps you can take. First, try to schedule a meeting with the person who is in charge of the program, such as a director. This will help to quicken the response to your message and help facilitate change. Be sure to bring these formal guideline documents with you to help build your case: the CDC’s updated guidelines and the official DOJ/ADA letter to schools regarding hepatitis B discrimination. You can even highlight the sections that apply to your case. Hopefully, the school will realize their mistake and make the necessary changes to their policy!
If the school refuses to acknowledge your lawful protections, you can reach out to us at info@hepb.org and we will assist you. You can also file a formal complaint with the DOJ.


 Phase 3 clinical trials have been announced for two drugs,
Phase 3 clinical trials have been announced for two drugs, 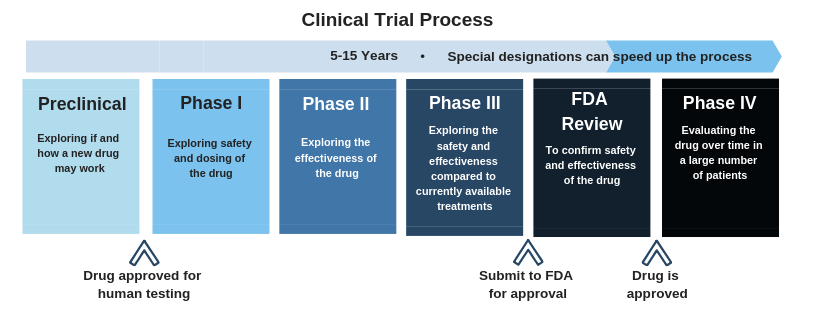 Click here
Click here
 Both issues can impair the liver’s ability to function and filter out toxins that enter the body. They can also increase a person’s risk of developing liver cancer. Recently,
Both issues can impair the liver’s ability to function and filter out toxins that enter the body. They can also increase a person’s risk of developing liver cancer. Recently, 
 excited to partner with the
excited to partner with the 
 especially if you are uncertain about how they will react. However, it is extremely important! Even if you are using condoms, it is necessary to let your partner know your status before becoming intimate. Once you tell them, it will be a huge relief!
especially if you are uncertain about how they will react. However, it is extremely important! Even if you are using condoms, it is necessary to let your partner know your status before becoming intimate. Once you tell them, it will be a huge relief!  show love than by being supportive? If your partner is living with hepatitis B,
show love than by being supportive? If your partner is living with hepatitis B,
