Twenty years ago when I found out my daughter had chronic hepatitis B, I would’ve purchased any drug I could find to cure her. I asked her doctor if she could join a pediatric clinical trial for lamivudine. I just wanted her cured as soon as possible. Fortunately, cooler heads prevailed.
My daughter didn’t need treatment then, and she doesn’t need it today. Her doctor was wise enough not to try an antiviral with an unknown track record that was later found to cause high rates of drug resistance. It would have caused more harm than good.
When we want hard to believe in something—especially a medicine that is advertised to cure hepatitis B–we end up listening to our hearts and not our heads.
Many people touched by hepatitis B around the world don’t have an expert to be the voice of reason and wisdom when they hear about false, counterfeit, or untried treatments for hepatitis B. Sadly, there is a steady increase in false marketing claims on Facebook and other websites using testimonials and marketing ploys to sell a counterfeit hepatitis B cure to we who are vulnerable, frightened, and desperate for a quick cure.
We at the Hepatitis B Foundation know this all too well. The public can post on our Facebook and blog pages. Often, unscrupulous people pitching ineffective cures will try to post a personal claim endorsing some doctor’s or herbalist’s new cure. Here’s a recent, verbatim example of a post to our Facebook page:
“Just wanna express my moment of joy for (having) been cured from the deadly HEPATITIS B. I have been infected with the Disease over three years and already lost hope (because) I have already tried so many ANTIVIRAL treatment…. one day while making more research online, I came across a testimony of a patients Dr … cured from GENITAL HERPES and I decided to give the said doctor a call….”
As you might expect, the writer claims to have been miraculously cured by the doctor using an antiviral drug called hepantivir, for example. But this drug has no scientific credentials. It has never been studied or tested or reported on in medical journals. But “experts” promise it will cure hepatitis B for $800.
We at the foundation remove these posts as soon as we discover them. These herbal supplements and counterfeit drugs can look very official, with medical-sounding names and packaged to appear like true pharmaceutical products. The advertising often features a photo of a doctor to appeal to a local audience. But they’re fake, and some of these “products” can even make you sicker than before you started the alleged, miracle drug.
In 2013, a study by the United Nations Office on Drugs and Crime that focused on Africa and South-East Asia suggested the counterfeit drug market in Africa was worth about $4 billion (USD). A report found that in 2009, in Nigeria, 60 out of 225 (27 percent) antimalarial medications failed chemical analysis, and in Ghana, 14 out of 17 (82 percent) antimalarial drugs followed suit.
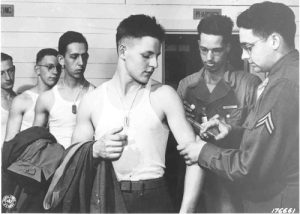
Their deceit is cruel and criminal, especially when it targets frightened people who may have no access to treatments or advice. In the U.S., drugs must be approved by the U.S. Food and Drug Administration. To win that approval, randomized, clinical trials that compare outcomes of treated patients to untreated patients (the control group), are needed to prove a drug actually does helps people. This is the gold standard of medical evidence.
That careful FDA review does not, however, apply to herbal supplements. One day, some of these supplements may indeed be found to have beneficial effects to protect the liver against hepatitis B after rigorous study and experiments. But that research hasn’t happened yet.
The U.S. National Institutes for Health has published a directory about what scientific research has discovered about common herbal supplements. Probably the most popular herbal supplement pitched as a liver remedy is milk thistle, and its extract silymarin. The NIH milk thistle report found, “Previous laboratory studies suggested that milk thistle may benefit the liver by protecting and promoting the growth of liver cells, fighting oxidation (a chemical process that can damage cells), and inhibiting inflammation. However, results from small clinical trials of milk thistle for liver diseases have been mixed, and two rigorously designed studies found no benefit.”
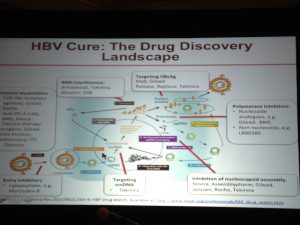
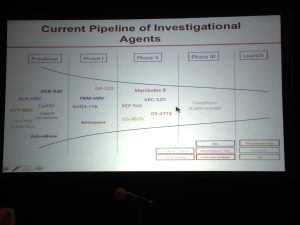
A true scientific evaluation is what we need to hear, even when we desperately want milk thistle or another supplement to be the cure. There is no magic bullet that is going to cure hepatitis B. It is a complex infection with no cure at this time. Experts are making great strides and hope to find a cure in the next few years, but now, this is the time to let our heads make healthcare decisions, instead of our vulnerable and hopeful hearts.
So be patient. Don’t fall for false promises, even when they’re accompanied by professional-looking photographs and emotional testimonials. If it sounds too good to be true, it probably is.
More information about counterfeit medications:
Quality Matters: Battling the Epidemic of Illegal Online Drug Sellers and Counterfeit Medicines Of the 35,000-50,000 active online drug sellers, 97 percent do not comply with U.S. laws and 50 percent of medicines sold online are fake or counterfeit, according to the Alliance for Safe Online Pharmacies (ASOP Global), an international non-profit headquartered in Washington, D.C. with operations in Europe and Asia.
These counterfeit medications are often manufactured in unsafe conditions; contain too little, too much or no active pharmaceutical ingredients; and, in many cases, have been found to contain dangerous substances like floor wax, rat poison, concrete, chalk, boric acid, road tar, paint, anti-freeze, and other toxins. This means that consumers worldwide are just a click away from buying products that may cause harm, treatment failure or even death. Read more…
Fight the Fakes Campaign: Fight the Fakes is a campaign to raise awareness about the dangers of fake medicines. The campaign gives a voice to those who have been personally impacted and shares the stories of those working to put a stop to this threat to public health. It seeks to build a global movement of organizations and individuals who will shine light on the negative impact that fake medicines have on people around the globe and to reduce the negative consequences on individuals worldwide.
As part of this effort, Fight the Fakes is collecting and sharing the stories of those who are impacted by fake medicines and are speaking up. The website also serves as a resource for organizations and individuals who are looking to support this effort by outlining opportunities for action and sharing what others are doing to fight fake medicines.