Welcome to the Hepatitis B Research Review! This monthly blog shares recent scientific findings with members of Baruch S. Blumberg Institute (BSBI) labs and the hepatitis B (HBV) community. Technical articles concerning HBV, Hepatocellular Carcinoma, and STING protein will be highlighted as well as scientific breakthroughs in cancer, immunology, and virology. For each article, a brief synopsis reporting key points is provided as the BSBI does not enjoy the luxury of a library subscription. The hope is to disseminate relevant articles across our labs and the hep B community.
This paper from the University of Duisburg-Essen in Germany shows that hepatocytes infected with HBV exhibit innate immune signaling via the pattern precognition receptor (PRR) Toll-Like Receptor 2 (TLR2). The adaptive immune response to HBV infection is well characterized and is broken into phases based on serological testing of antibodies produced against the virus. However, whether HBV infection triggers an innate immune response has remained controversial, with the long-held belief being that HBV evades the innate immune system as a “stealth virus”. Contrary to this view, studies of acute HBV infection in patients have indicated an early, innate immune response to HBV characterized by a natural killer (NK) cell response. Toll-like receptors (TLRs) are a class of membrane-bound receptor proteins which play a key role in innate immunity by recognizing foreign pathogens and activating inflammatory signaling cascades. A previous publication from this group has demonstrated that primary human hepatocytes (PHHs) can be stimulated through the TLR proteins TLR1-9. In this paper, PHHs from human donors were infected with HBV ex vivo. Then, expression of the innate immune cytokines Interleukin 1 Beta (IL1B), Interleukin 6 (IL6), and Tumor Necrosis Factor Alpha (TNFα) were measured by quantitative, reverse-transcription polymerase chain reaction (qRT-PCR). HBV-infected PHHs showed greatly increased expression of these genes at three hours after infection compared to mock-infected and not treated PHHs. Additionally, immunocytochemical staining revealed translocation of the transcription factor nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) to the nuclei of HBV-infected PHHs, indicating a cytokine response. Next, to characterize the innate immune response caused by HBV infection, a DNA microarray was used. Here, PHHs were either infected with HBV or treated with a known TLR ligand such as Pam3Cys (TLR2 agonist) or poly(I:C) (TLR3 agonist). Then, RNA was extracted from the cells and converted through a complementary DNA (cDNA) intermediate into biotin-labeled anti-sense RNA (aRNA) which was then hybridized to a Human Genome U219 Array Plate. This plate, coated with over 530,000 DNA probes representing over 20,000 human genes served as a scaffold for complementary base-pair binding of the aRNAs derived from the cells. Once bound to the microarray, the biotin-labeled aRNAs were detected by staining with streptavidin phycoerythrin, resulting in a fluorescent signal wherever complementary base-paring occurred. This microarray analysis revealed which specific inflammatory genes were up-regulated in the PHHs by each stimuli. Gene expression signals which were induced by HBV infection were compared with those induced by the TLR agonists. The gene expression profile of HBV-infected PHHs was most similar to that of PHHs treated with the TLR2 agonist Pam3Cys. This data indicates that HBV infection induces a TLR2-like innate immune response. Importantly, no expression of interferon-stimulated genes (ISGs) was detected in the microarray analysis. Finally, PHHs were pre-treated with neutralizing antibodies against TLR2 (nABTLR2) prior to infection with HBV. HBV-mediated induction of IL1B, IL6 and TNF was significantly reduced by nABTLR2 pre-treatment and conversely, HBV replication was increased. In summary, this paper shows that PHHs exhibited an innate immune response to HBV infection via the TLR2 pathway. The group suggests that this response is one of the body’s first steps leading to HBV clearance. Furthermore, in the discussion section the group indicates that the HBV surface antigen (HBsAg) is likely the protein component of HBV which activates TLR2 upon infection. This finding may help in the development of strategies to cure chronic HBV infection.
- Hepatitis B virus-triggered PTEN/β-catenin/c-Myc signaling enhances PD-L1 expression to promote immune evasion
– American Journal of Physiology-Gastrointestinal and Liver Physiology
This paper from Wuhan University in China reports that HBV infection can increase the expression of Programmed Death Ligand 1 (PD-L1) on the surface of infected hepatocytes, allowing them to escape destruction by the adaptive immune system. PD-L1 is the binding partner of Programmed Death 1 (PD-1), an immune checkpoint protein on the surface of T cells. The expression of PD-L1 on cell surfaces allows for their recognition by circulating T cells as part of the body and not an outside threat. This interaction is important for the prevention of autoimmune disorders in which the immune system attacks healthy cells of the body. However, PD-L1 is commonly over-expressed in a number of cancers and is a hallmark of especially aggressive cancers. PD-L1 expression on cancer cells allows them to neutralize T cells which specifically target them. This is one example of an “immune-escape” strategy exhibited by cancers. Accordingly, PD-L1 and PD-1 are the target of a number of FDA approved immunotherapies for cancer including the PD-L1 inhibitors Tecentriq, Bavencio, and Imfinzi and the PD-1 inhibitors Keytruda, Opdivo, and Libtayo. These drugs are some of the first in their class in that they are not small molecules, but are recombinant, monoclonal antibodies. Phosphatase and tensin homologue deleted on chromosome 10 (PTEN) is a tumor suppressor which is mutated or deleted in many human cancers. PTEN is a phosphatase, a protein which dephosphorylates other molecules. This group has previously shown that PTEN plays a role in antiviral innate immunity. Therefore, they wanted to see if PTEN also regulates the adaptive immune response in the context of HBV infection. First, they used immunohistochemical staining of patient liver tissues to compare the levels of PTEN and PDL-1 in patients chronically infected with HBV vs healthy controls. There was a reduced staining of PTEN and a heightened staining of PD-L1 in chronic HBV tissues compared to controls. The group then found a similar correlation using immunofluorescence, qPCR and Western blotting of HepG2 cells vs HepG2.2.15 (HBV-producing) cells. They also transfected HepG2 cells and infected mice via hydrodynamic injection with an HBV-containing vector (pHBV1.3) or an empty vector control (pUC18) and then performed qPCR and/or Western blotting. In all systems, HBV infection/production induced a reduction of PTEN and an increase in PD-L1 expression. Then, in order to elucidate this phenomenon further, a PTEN-expressing plasmid was transfected into HepG2.2.15 cells, which resulted in a reduction in PD-L1 mRNA and protein. Conversely, PTEN knockdown in HepG2.2.15 cells resulted in a two-fold increase in PD-L1 mRNA and protein expression. These results show that HBV inhibits PTEN expression which in turn causes up-regulation of PD-L1. Next, the group transfected HepG2 and Huh7 cells with a number of constructs conferring individual HBV proteins. They found that HBV X protein (HBx) and HBV polymerase (HBp) reduced PTEN expression more than any other HBV protein components. Next, the group analyzed how HBV production in hepatocytes affected human T cells grown in co-culture. Jurkat T cells were co-cultured with either HepG2 or HepG2.2.15 cells and then analyzed by flow cytometry. Jurkat T cells grown alongside the HBV-producing HepG2.2.15 cells had a higher incidence of apoptosis, a higher expression of PD-1, and less Interleukin-2 (IL-2) secretion than those grown alongside HepG2 cells. This result indicates that HBV-infected hepatocytes suppress local T cell responses by PD-L1/PD-1 signaling. Finally, the group used a mouse model of HBV infection to show that PTEN over-expression promotes HBV clearance in vivo. This paper shows that PD-L1, a highly studied drug target implicated in the immune-escape of cancers is also up-regulated by HBV infection. Furthermore, the HBV proteins responsible for this up-regulation are HBx and HBp. This finding may help in the development of immunotherapies to treat chronic HBV infection. Perhaps FDA approved PD-L1 or PD-1 inhibitors may be used in conjunction with interferon alpha treatment or HBV antivirals to boost the immune response against HBV-infected hepatocytes.
- Highly efficient and tumor-selective nanoparticles for dual-targeted immunogene therapy against cancer
–Science Advances
This paper from National Tsing Hua University in Hsinchu, Taiwan reports the design and testing of nanoparticles which selectively confer immunogene therapy to hepatocellular carcenoma (HCC) cells. Nanoparticles are very small (1-1000nm) particles which have become an attractive novel drug candidate in recent years. The use of nanoparticles as medicine would enable the customizable delivery of DNA, RNA, or protein payloads to cells. The novel nanoparticles presented here deliver both a small interfering RNA (siRNA) against the Programmed Death Ligand 1 (PD-L1) gene as well as a plasmid DNA (pDNA) encoding the cytokine Interleukin 2 (IL-2). The strategy behind the nanoparticles’ design is to both inhibit an immunosuppressive gene (PD-L1) and up-regulate an immunostimmulatory gene (IL-2) in tumor cells. Delivery of such genes to tumor cells would make them more vulnerable to destruction by circulating cytotoxic T cells (CD8+ T cells). This type of approach is needed, because many advanced tumors create an immunosuppressive tumor micro-environment (TME) rendering many cancer treatments ineffective. The nanoparticles presented here are referred to as tumor-targeted lipid dendrimer-calcium phosphate (TT-LDCP) nanoparticles. The nanoparticles consist of a core of calcium phosphate, thymine-capped polyamidomine (PAMAM) dendrimers, siRNA, and pDNA. This core is coated with an inner lipid called DOPA and outer leaflet lipids DOPC, DOTAP, and DSPE-PEG. The nanoparticle is then tagged with SP94 (SFSIIHTPILPL), a polypeptide which selectively binds to HCC cells but not healthy hepatocytes. Dendrimers are repeatedly-branching molecules which exhibit a sphere-like shape. PAMAMs are the most well-characterized class of dendrimers, consisting of branching amide and amine groups. The calcium phosphate and PAMAM dendrimers in the core of the TT-LDCP nanoparticle promote endosomal escape of the nucleic acid payload. Additionally, this group shows that the PAMAM dendrimers in TT-LDCP nanoparticles also activate the STING pathway. The group showed that STING was activated by treating mouse HCC cells HCA-1 with complete nanoparticles or those lacking the dendrimers. Cells treated with complete nanoparticles showed, by Western blot a higher level of both TBK1 and IRF3 phosphorylation than those treated with incomplete nanoparticles. Those cells treated with complete nanoparticles also displayed heightened transcription of the STING-triggered proinflammatory genes Ifnb,Ccl5, and Cxcl10 as measured by qPCR. Furthermore, the group showed that treatment using their nanoparticles of mice bearing orthotopic HCC implants resulted in dendritic cell maturation in those animals, regardless of the identity of the genes delivered. These results indicate that the dendrimers used in the TT-LDCP nanoparticles not only serve for efficient delivery of nucleic acids, but also as adjuvants that stimulate the STING pathway and activate tumor-infiltrating dendritic cells. This publication gives a glimpse into what future therapies for cancer may look like. The nanoparticle designed by this group is unique in that it has multiple functionalities: selectively targeting HCC cells, inhibiting PD-L1 expression, inducing IL-2 expression, and activating the STING pathway. Such a complex design is bound to require fine tuning before it can become a medicine. But a multi-target immunotherapeutic such as this may be exactly what is needed to help the body fight against aggressive, immunosupressive tumors.
Lay Summary:
This month, the innate immune system was the focus of HBV research. Scientists hope to find how the innate immune system interacts with HBV during viral infection and proliferation. Doing so will shed light on host factors which lead to chronic infection and inform antiviral strategies. Notably, this month a human protein, MX2 was found to have potent anti-HBV activity by preventing cccDNA formation. Also, a microRNA encoded by HBV called HBV-miR-3 was found to activate the human innate immune system to limit HBV replication. This month, a paper studying woodchuck hepatitis virus (WHV) traked activation of the innate immune system as well as he adaptive immune system in an acute infection model. Also this month, concerning hepatocellular carcenoma (HCC), the alternative splicing of mRNA in tumors was found to vary in HCC patients based upon their risk factor (HBV, HCV, or alcohol). Finally, a review was published this month concerning STING, an innate immune protein which is not activated by HBV infection but which may prove a valuable tool for cancer treatment.
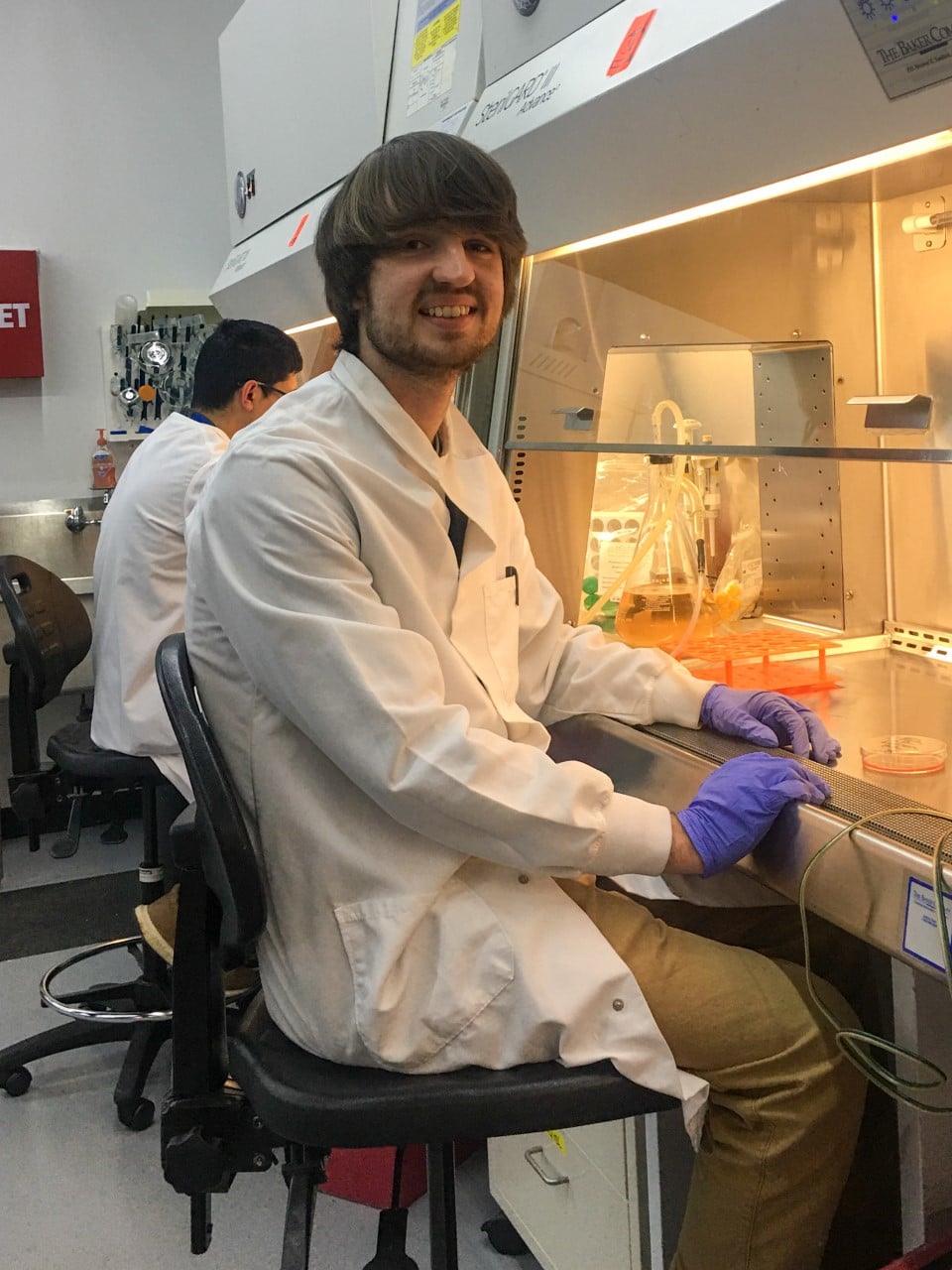
Meet our guest blogger, David Schad, B.Sc., Junior Research Fellow at the Baruch S. Blumberg Institute studying programmed cell death such as