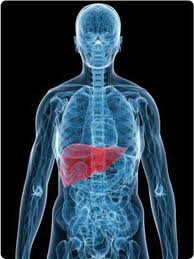
The American College of Gastroenterology wrapped up its annual meeting in Washington, D. C. this week. A few of the topics discussed apply to those living with hepatitis B or the prevention of HBV and other blood-borne pathogens.
The American College of Gastroenterology wrapped up its annual meeting in Washington, D. C. this week. A few of the topics discussed apply to those living with hepatitis B or the prevention of HBV and other blood-borne pathogens.
Hepatitis Transmission Risk Needs to be Studied in Nail Salons and Barbershops is a press release that discusses a new analysis presented at this year’s annual ACG conference. It looks at your favorite nail and hair salon and barbers shop and discusses the risk of infectious disease transmission. Since HBV is more infectious than both HIV and HCV, it would seem the transmission of HBV might be higher. There is not a great deal of conclusive data out there, but they agree it warrants further study.
Practically speaking, certain shop activities could provide a vehicle for transmission of HBV and other blood-born pathogens if adequate precautions are not followed. Fortunately there is a safe and effective vaccine for HBV, but not for HCV and HIV. No one wants an infectious disease, and if you are living with HBV, you don’t want to be co-infected with another viral agent.
For those living with HBV, it is recommended that personal care items such as nail files, clippers, and tweezers NOT be shared. At your favorite nail salon, it is possible that “tools of the trade” such as nail files, cuticle pushers, nail buffers, brushes, clippers, are not single-use, or properly disinfected. Microscopic droplets of blood could readily transmit infectious disease. Even items such as finger-bowls and foot basins need to be properly disinfected.
At this time, there are no OSHA or CDC guidelines for infection control practices for nail and hair salons, and barbershops. They are all state regulated. Please check out this guide to regulations for nail salons, listed state-by-state. Unfortunately there was not a similar guide pulled together for hair salons and barber shops.
It is important to know what is expected at your nail salon in your state, and determine whether or not you are adequately protected. The next concern is whether or not disinfection practices are followed by the shop, and enforced by state inspectors. You should be able to figure some of this out by spending a little time in the shop, or by asking. If you feel like you’re getting a great deal at a discount nail salon, think again of the hidden risks with a shop that does not disinfect, or use single-use items. Many shops will maintain personal nail care tools for individual customers. This is the way to go – whether you bring in your own tools or store them at the shop.
Here’s what you can do to help protect yourself and others:
- Bring your own tools.
- If you have cuts, bug bites, or a skin infection, do not get a manicure or pedicure.
- Is there an autoclave in the shop? If not, are the instruments properly sanitized or disposed of? How about the foot spas? Are they disinfected in between clients (10 minute cycle) and is the footbath intake filter cleaned weekly? You’re probably not sure, so ask!
- Do NOT shave your legs immediately prior to a pedicure appointment. Shaving increases the risk of infection
- Use your own cutting and filing tools. Some nail salons will keep tools of regular customers on-site.
- Avoid credo blades or sharp instruments used for shaving calluses.
- Reconsider cutting your cuticles
- If the shop is clearly dirty, leave. If the “tools of the trade” look dirty or messy, leave. This applies to both hair and nail salons or barbershops.
Your goal is to avoid shop activities that increase the risk of infectious disease transmission. Basically this means the dispersal of any microscopic blood or body fluids. Accidents happen, and many are unaware they have a blood-borne pathogen infection. You can also get a nasty bacterial and fungal infections, so a clean shop with proper disinfection practices is imperative for so many reasons.
The same thing goes for the hair salon and barber shop. Avoid obvious activities that might lead to the transmission of infectious disease. If the shop is poorly maintained, dirty, or disorganized, go somewhere else. If you are having problems with your scalp that causes scabs or bleeding, wait to get a haircut, but remember that others might not do the same. You want to be sure that hair care items are free of debris (hair and skin) and properly disinfected. This video from the Department of Regulatory Agencies for the state of Colorado (DORA) gives very thorough disinfection instructions, but I find it hard to believe that all of these procedures are being followed in all shops.
If you are a man, consider whether or not it is really wise to get a shave at your local barber. Many shops no longer perform this service, although it is more common in other cultures. If yours does provide a shave, and you partake, be sure the razor handle is properly sterilized between customers, with a new razor used for each. Razors are such an effective mode of HBV transmission, so be aware.
Keep in mind that if you have HBV and enjoy getting your nails done on a regular basis, or visit the hair salon regularly, please be aware of the fumes emitted from the various chemicals in nail and hair products. Many of these fumes are not liver-friendly, so if you must, please be sure to frequent a shop where there is good ventilation. Fortunately there are greener alternatives out there, but not all shops are using them. Good ventilation is key.
When my kids were little, I discouraged all nail polish for my little nail-biter, and toluene free polish when I relented. Now there are better alternatives for everyone, so take advantage of them.
So next time you step into your neighborhood nail or hair salon or barbers shop, take a look around and make sure you are satisfied with the conditions. There are some form of infection control and disinfection practices in place, but are they being followed? You might just have to ask!