
The annual Hep B United Summit, organized by the Hepatitis B Foundation, convenes in Washington D.C. from Wednesday, July 24 through Thursday, July 25. The theme of the 2019 summit is Eliminating Hepatitis B: Local Change, Global Impact. National and local coalition partners, experts, stakeholders, and federal partners will meet to discuss how to increase hepatitis B testing and vaccination and improve access to care and treatment for individuals living with hepatitis B.
You can watch many of these sessions on Facebook Live. You can also follow the conversation at the Summit on Twitter with #Hepbunite19!
Facebook Live video streaming is available to all Pages and profiles on Facebook. Check out the agenda below and go to the Hep B United Facebook Page to view the live broadcast. Some breakout sessions may be broadcast from the Hepatitis B Foundation Facebook Page. Sessions will also be available following the broadcast for those who are not able to join us live.
Here are the details on the sessions that will be broadcast on Hep B United’s Facebook Live unless noted otherwise:
Day 1 – Wednesday July 24:
8:00 – 9:00 AM: Welcome and Introductions
Tim Block, PhD, President & Co-Founder, Hepatitis B Foundation
Chari Cohen, DrPH, MPH, Co-Chair, Hep B United and Senior Vice President, Hepatitis B Foundation
Jeff Caballero, MPH, Co-Chair, Hep B United and Executive Director, Association of Asian Pacific Community Health Organizations (AAPCHO)
9:00 AM: CDC Division of Viral Hepatitis
Carolyn Wester, MD, MPH, Director, Division of Viral Hepatitis, Centers for Disease Control and Prevention
9:30 AM: The Path to a Hepatitis B Cure
Tim Block, PhD, President and Co-Founder, Hepatitis B Foundation
10:15 AM: Local Initiatives: Eliminating Hepatitis B Across the Lifespan
Moderator: Catherine Freeland, MPH, Public Health Program Manager, Hepatitis B Foundation
Panelists:
Moon S. Chen, MPH, PhD, Professor, University of California – Davis
Liz Tang, Health Care Access Specialist, and Farma Pene, Health Care Coordinator, New York City Department of Health & Mental Hygiene
Chelsie Porter, MPH, Prevention & Outreach Program Manager, Hepatitis Education Project
11:15 AM: Integrating Systems Level Changes to Eliminate Hepatitis B
Moderator: Chari Cohen, DrPH, MPH, Senior Vice President, Hepatitis B Foundation
Panelists:
Jeff Caballero, MPH, Executive Director, AAPCHO
Su Wang, MD, MPH, Medical Director, Center for Asian Health, Saint Barnabas Medical Center, Livingston, NJ
Richard Andrews, MD, Research Director, HOPE Clinic, Houston, TX
12:30 PM: Lunch Keynote Presentation
Center for Disease Analysis Foundation
Devin Razavi-Shearer, Hepatitis B/D Project Lead
1:45-3:00 PM BREAKOUT SESSIONS I
Innovative Strategies to Conduct HBV Education, Testing, and Linkage to Care
Discuss effective outreach strategies to conduct HBV education, testing, and patient navigation among high-risk communities.
Moderator: Sherry Chen, MPH, CHES, CDC Division of Viral Hepatitis
Panelists:
Paul Lee and Ohkyun Ko, Korean Community Services, New York, NY
Chooson Byambaa & Tuya Lkhaijav, Hepatitis B Initiative of Washington, DC
Alia Southworth, Asian Health Coalition, Chicago, IL
Increasing HBV Provider Education (HepBFoundation Facebook)
Join the National Task Force on Hepatitis B to discuss the development of provider education tools to manage chronic hepatitis B in the primary care setting.
Facilitators: Amy Trang, PhD, MEd, Administrator and Richard Andrews, MD, Co-Chair, National Task Force on Hepatitis B
3:15 PM – 4:45 PM BREAKOUT SESSIONS II
Local, National, and Global Efforts to Increase HBV Testing and Education Among African Communities (HepBFounation Facebook)
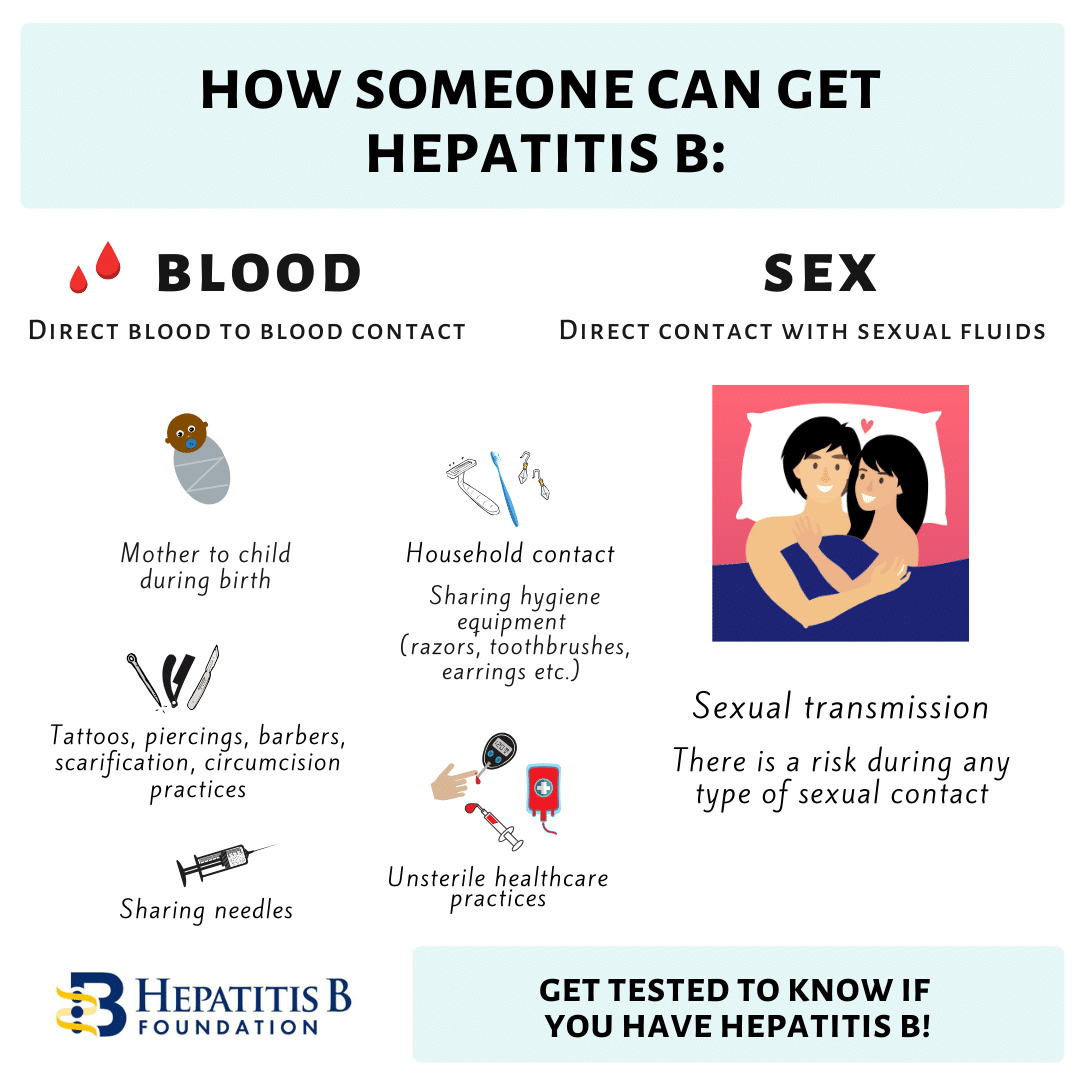
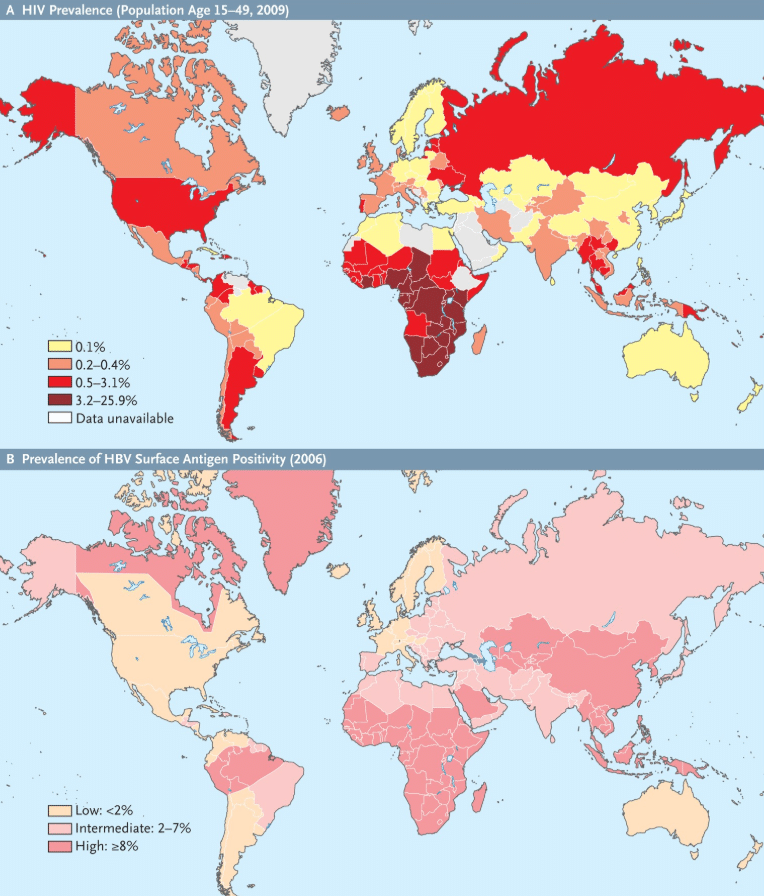
Discuss pioneering efforts and strategies to raise awareness and promote testing in African communities, whose hepatitis B burden rivals that of Asian Americans. Learn tips for education and how your organization can begin or expand current work.
Moderator: Cynthia Jorgensen, DrPH, CDC Division of Viral Hepatitis
Panelists:
Oni Richards, African Family Health Organization, Philadelphia, PA
Chioma Nnaji, Multicultural AIDS Coalition, Boston, MA
Sierra Pellechio, CHES, Hepatitis B Foundation
Catherine Freeland, MPH, Hepatitis B Foundation
Combating HBV-Related Stigma and Discrimination
Discuss the impact of HBV-related stigma and development of policies to combat institutional discrimination.
Moderator: Maureen Kamischke, Hepatitis B Foundation
Panelists:
Vrushabh Shah, MPH, NASTAD
Nadine Shiroma, Alexa Canizzo,, Hepatitis B Foundation
Day 2 – Thursday July 25
8:30 AM: National Action Plan to Eliminate Hepatitis B
Carol Jimenez, Deputy Director for Strategic Initiatives, Office of Infectious Disease and HIV/AIDS Policy, U.S. Department of Health and Human Services
9:00 AM: Global Efforts to Eliminate Hepatitis B
Su Wang, MD, MPH, President-Elect, World Hepatitis Alliance
9:30 AM: Patients Driving Change: #justB Storytelling Campaign
Moderator: Rhea Racho, MPAff, Public Policy & Program Manager, Hepatitis B Foundation
#justB Storytellers Panel: Cuc Kim Vu, Peter Vo, Bright A., Xuan Phan, and Jacki Chen
11:00 AM: Improving Access to Hepatitis B Treatment
Panelists:
Michaela Jackson, MS, Public Health & Outreach Program Coordinator, Hepatitis B Foundation
Alyssa Gallipani, PharmD, BCACP, Ambulatory Care Specialist and Clinical Assistant Professor of Pharmacy Practice, RWJ Barnabas Health & Fairleigh Dickinson University
Carl Schmid, MBA, Deputy Executive, Director, The AIDS Institute
12:15 PM:
EliminatingTuberculosis in Asian American Communities
Nickolas Deluca, PhD, Branch Chief, Communications, Education, and Behavioral Studies, Division of TB Elimination, Centers for Disease Control and Prevention
1:00 PM: HBU Coalition Strategies
Facilitator: Amy Trang, PhD, Administrator, National Task Force on Hepatitis B
Not able to join the sessions with Facebook Live? Follow the conversation on Twitter using the #Hepbunite19 hashtag. Follow the events, retweet and engage with event attendees and help us raise hepatitis B awareness in the U.S. and around the globe. We’ll also be posting on twitter during our Advocacy Day, Tuesday, July 23rd.
World Hepatitis Day is July 28th, and this Summit is an opportunity to share with the world what we’re doing to help those living with hepatitis B in our communities. Other popular hashtags for World Hepatitis Day, and to raise hepatitis B awareness, include: #NOhep, #KnowHepB, #WorldHepatitisDay, #WorldHepDay, #WHD2019, #FindTheMissingMillions #hepatitis, #hepatitisB, #HBV, #hepB, #justB. Connect with, follow and engage with fellow partners and advocates on twitter to keep the hep B conversation going during the Hep B United Summit, World Hepatitis Day events, and beyond.
Check out: @AAPCHOpolicy, @aidsadvocacy, @alex_daleks, @aphfsd, @APPEALhealth, @AVACNow, @bentheactivator, @CAHE_AHC, @catherineafree, @CDAFound, @cdchep, @CDC_TB, @ChoosonB, @hepBaware, @HBIDC, @HepBFoundation, @HepBpolicy, @HepBUnited, @HepBUnitedPhila, @hepdconnect, @HepEduProject, @HepFreeHawaii, @hepfreeNYC, @HHS_ViralHep, @HOPECHC, @iwgroup, @jacki0362, @jeffaapcho, @KCSNY, @kmoraras, @Liz98223514, @nirahjohnson, @NYU_CSAAH, @ponnivp, @randrews98, @RheaRacho, @swang8 @tuugiil73
Missing from the list? Contact the Foundation at info@hepb.org to be added.
We’re having a World Hepatitis Day exhibit on Capitol Hill in the Rayburn Building Foyer, Friday, July 26th from 10 am to 3 pm. We’ll be asking legislators and partners how they plan to “Find the Missing Millions” living with hepatitis B.
Visit the Hep B United and Hepatitis B Foundation websites for more information about hepatitis B and related programs.


 covered medications, or
covered medications, or 
 Join
Join