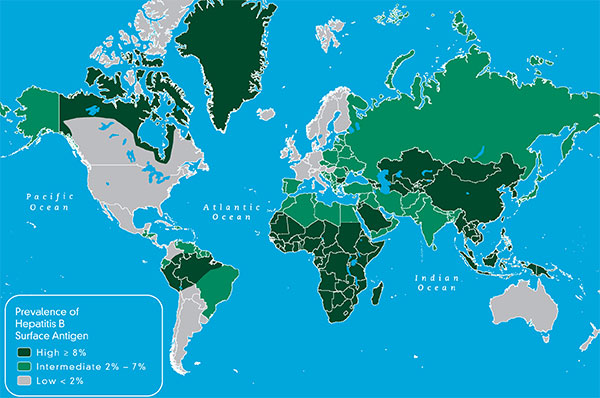
According to the World Health Organization (WHO), liver cancer is the second most common cancer in the world, leading to 788,000 annual deaths worldwide. Most liver cancer cases occur in developing countries. More than 80 percent of these cancers are found in sub-Saharan Africa and Eastern Asia where more than 20 of every 100,000 people will suffer and die from liver cancer. However, liver cancer is alarmingly on the rise in developed countries, as well. In a recent study, researchers from The American Cancer Society found that liver cancer is the fastest-growing cause of cancer deaths in the United States. Only 20 percent of people diagnosed with liver cancer survive beyond five years, and the number of deaths have doubled since the mid-1980s, and they are expected to continue to rise.
Why is liver cancer growing in most of the world? There are many risk factors for liver cancer, but chronic hepatitis B accounts for up to 60% of liver cancer and is the most common risk factor for this type of cancer. People who are chronically infected with hepatitis B are 100 times more likely to develop liver cancer compared to those who are not. The hepatitis B virus attacks the liver directly and repeatedly over time. This can lead to liver damage and scarring of the liver (or cirrhosis); which greatly increases the risk of liver cancer.
Sometimes, people with hepatitis B can develop liver cancer even when they do not have cirrhosis. There are a number of complicating factors which can increase the risk of liver cancer including traits specific to the virus and the person and their health status, which should be discussed with a liver specialist to determine when you should initiate screening.
 How many years have you had hepatitis B? The longer you’re infected, the higher your risk of liver cancer.
How many years have you had hepatitis B? The longer you’re infected, the higher your risk of liver cancer.
What is your gender? Men are considered at higher risk of liver cancer and may be screened starting at an earlier age because they may be more likely to smoke, drink alcohol, have more “active” hepatitis, and higher iron stores—all of which increase cancer risk. Estrogen is believed to protect pre-menopausal women against liver cancer.
Have you had a high viral load (HBV DNA) after age 30? Having a viral load exceeding 2,000 international units per milliliter (IU/mL) is associated with a higher risk of liver cancer even if you have no other signs of liver damage.
Do you have a family history of liver cancer? If an immediate family member has had liver cancer, this greatly increases your risk.
Are you overweight, or have you been diagnosed recently with type 2 diabetes? A fatty liver and/or diabetes increase your risk of liver damage and cancer dramatically when you’re also infected with hepatitis B.
Do you have hepatitis B virus genotype C or core/precore viral mutations? Originating in Asia, this hepatitis B strain is associated with loss of the hepatitis B e antigen (HBeAg) later in life. That means you may have had a high viral load and liver damage for a longer period than people with genotypes who clear HBeAg at a younger age. Having core or precore mutations in your HBV also increase liver cancer risk.
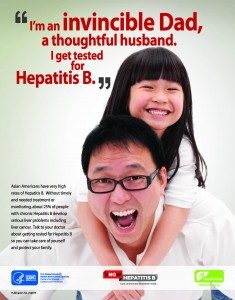
If you are living with chronic hepatitis B and are concerned about liver cancer, there are steps you can take. Working with a good health care provider to manage your hepatitis B is important, as is having a healthy lifestyle. Talk to you doctor about your risk, and about getting screened for liver cancer at least annually – early detection saves lives!
To commemorate Liver Cancer Awareness Month this October, help us spread the word about the link between hepatitis B and liver cancer! You can also join our Twitter Chat on Thursday, October 12th at 2:00pm – along with our partners CDC Division of Viral Hepatitis, and the National Alliance of State and Territorial Aids Directors (NASTAD). To join the chat, use the hashtag #liverchat. For more information, visit our blog post.
Remember to talk to your doctor about the risk factors for liver cancer, and if you have hepatitis B, ask to get screened for liver cancer. For more information about liver cancer visit the Liver Cancer Connect website.











 The news was all good. His children had been immunized and were fine, he was not infected and was immediately immunized. Today, we are all doing fine, including our daughter.
The news was all good. His children had been immunized and were fine, he was not infected and was immediately immunized. Today, we are all doing fine, including our daughter.