Great blog written by Corinna Dan, RN, MPH, Viral Hepatitis Policy Advisor, Office of HIV/AIDS and Infectious Disease Policy, HHS , discussing the strategy to eliminate perinatal transmission of hepatitis B in the U.S. In many parts of the world, transmission from an HBV infected mother to her baby is the most common mode of transmission. If you are a pregnant woman, please ask your doctor to screen you for hepatitis B. If you learn you have hepatitis B, talk to your doctor to be sure your baby receives appropriate prophylaxis within 12 hours of birth so you can break the cycle of transmission from mother to baby. Happy Mothers Day!
Great blog written by Corinna Dan, RN, MPH, Viral Hepatitis Policy Advisor, Office of HIV/AIDS and Infectious Disease Policy, HHS , discussing the strategy to eliminate perinatal transmission of hepatitis B in the U.S. In many parts of the world, transmission from an HBV infected mother to her baby is the most common mode of transmission. If you are a pregnant woman, please ask your doctor to screen you for hepatitis B. If you learn you have hepatitis B, talk to your doctor to be sure your baby receives appropriate prophylaxis within 12 hours of birth so you can break the cycle of transmission from mother to baby. Happy Mothers Day!
Eliminating Perinatal Transmission of Hepatitis B: More Than Just a Test
Hepatitis B in the U.S.
Nationally, new hepatitis B infections have been reduced by 82% since 1991 because of the availability of safe and effective vaccines, as well as improved prevention in healthcare settings. The Centers for Disease Control and Prevention (CDC) estimates that 1.4 million Americans are living with chronic hepatitis B infection. Unfortunately, many of these people became infected before the widespread availability of the hepatitis B vaccine in the early 1980s. Most are unaware of their infection, which places them at greater risk for severe complications of the disease, and for transmitting the virus to others. For women of childbearing age, this lack of awareness also increases the likelihood of transmitting hepatitis B to their infants.
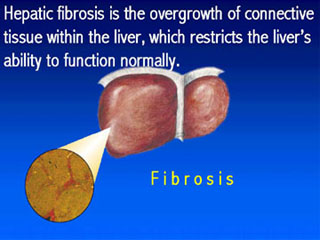
Perinatal hepatitis B – spread from an infected mother to her infant at the time of birth – is estimated to account for 800-1,000 new infections each year in the United States. Unfortunately, this number of annual new, preventable infections has remained unchanged in recent years, which is why the elimination of mother-to-infant transmission of hepatitis B is one of the main goals of the Action Plan for the Prevention, Care & Treatment of Viral Hepatitis. As the Plan observes, the persistent annual number of perinatal hepatitis B cases is particularly concerning because approximately 90% of HBV-infected newborns develop chronic infection; up to 25% of these children will die of cirrhosis, liver failure, or liver cancer later in life.
Tackling Perinatal Hepatitis B
To achieve the goal of eliminating perinatal HBV, the Action Plan calls for the provision of postexposure prophylaxis (i.e., hepatitis B immune globulin and hepatitis B vaccine) to all infants born to HBV-infected women, a strategy consistent with the recommendations of the Advisory Committee on Immunization Practices (ACIP) in its “Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus Infection in the United States.” This recommended treatment is to be provided within 12 hours of birth followed by timely completion of the rest of the three-dose hepatitis B vaccine series, to prevent the infant from contracting hepatitis B. The Action Plan and ACIP also observe that care coordination is needed to ensure that infants born to HBV-infected women receive the services needed to protect them against hepatitis B.
A vital partner in these efforts to eliminate mother-to-infant transmission of hepatitis B is CDC’s Perinatal Hepatitis B Prevention Program (PHBPP) which supports activities in all 50 states, six cities, and five territories. The PHBPP was established in collaboration with state/local health departments and healthcare providers to promote use of the available tools – prenatal testing and vaccines – to reduce perinatal HBV transmission. The program works to identify pregnant women who are infected and provides case management services to ensure that infants receive the appropriate vaccines after birth to help prevent perinatal transmission. This program has been successful, ensuring that 95% of the identified infants born to infected mothers and case managed by the program received hepatitis B immune globulin and the first dose of hepatitis B vaccine within one day of birth and 83% of these infants complete the hepatitis B series by 12 months of age. In addition, whenever possible, the mother is counseled about hepatitis B and encouraged to talk with her healthcare provider for a full HBV evaluation. The program also seeks to identify household and sexual contacts of women who test HBV-positive – CDC reports that in 2011 the programs identified 9,681 such contacts – providing prevention information and recommending screening.
Despite these successful outcomes, challenges remain; the PHBPP estimates it identifies and case manages only about half of the expected births to hepatitis B infected women annually. Although hepatitis B screening is recommended for all pregnant women as part of routine prenatal care, not all women are screened. Some women do not seek or remain in prenatal care. In other cases, even when HBV screening occurs, health departments are not informed of screening results that reveal a pregnant woman is infected with hepatitis B – in some cases this is because such reporting is not required in that jurisdiction, in other cases it is an error or oversight. Under these circumstances, the health department cannot connect the expectant mother and her family to the services available through the PHBPP.
Another key support to efforts to eliminate perinatal HBV transmission is the implementation of provisions of the Affordable Care Act that will help improve prenatal hepatitis B screening. Under the Affordable Care Act, the hepatitis B test for pregnant women is among the Preventive Services that new health insurance plans issued after September 23, 2010 are required to cover without the consumer having to pay a copayment or co-insurance or meet her deductible. By making hepatitis screening more widely accessible and eliminating cost barriers, the healthcare law will also help bring us closer to the Action Plan’s goal of eliminating perinatal transmission of HBV.
In order to further reduce the number of infants who are perinatally infected with hepatitis B, healthcare providers, practices, and hospitals that care for pregnant women need to increase awareness and efforts to accurately report hepatitis B-infected pregnant women and refer the families to the PHBPP.
What Can Healthcare Providers Do?
Healthcare providers play a key role in eliminating perinatal hepatitis B. Steps that healthcare providers can take include:
- Ensure that your practice is collaborating with the public health department to report women who are chronically infected so that their infants can benefit from case management. The CDC viral hepatitis reporting form [PDF 46KB] is available online.
- Educate your patients about hepatitis B and listen to their concerns; the CDC has great educational materials available for patients.
- Work with your local hospitals and birthing centers to ensure that they are following recommended policies and procedures.
- Reach out to your state/local Perinatal Hepatitis B Coordinator if you have any questions or need additional assistance to implement the CDC recommendations.
What Can Pregnant Women Do?
- Ask your healthcare provider if you were tested for hepatitis B and what the result of the test was.
- Learn more about hepatitis B to make sure your new infant receives the preventive services needed to prevent hepatitis B infection at birth and throughout your child’s life.
- If you learn that you are living with hepatitis B, check out the CDC’s frequently asked questions and talk with your healthcare provider to find out what you should do to stay healthy and ensure that you will be there to nurture and watch your child grow.
On this Mother’s Day during Hepatitis Awareness Month, please take the opportunity to learn more about hepatitis B and what steps you can take to realize the goal of eliminating mother-to-infant transmission of this preventable disease.
Please link to the original article if you would like to listen to this blog in it’s entirety.