
By Christine Kukka
Don’t know your hepatitis B status? Get tested. Worldwide an estimated 90 percent of people with chronic hepatitis B don’t know they’re infected. In the U.S. only 25% are aware of their infection. Unfortunately, many doctors won’t test you for hepatitis B unless you request the test. If you or your parents come from or live in a country with high rates of hepatitis B, or if you’ve been sexually active or have other risk factors , get tested. It could save your life.
Get tested for sexually-transmitted infections (STIs). More than half of us will have an STI in our lifetime, and in the U.S. about half of new hepatitis B infections are sexually-transmitted. Many doctors don’t test for STIs. In a national survey of U.S. physicians, fewer than one-third routinely screened patients for STIs. To make matters worse, many women are afraid to talk to doctors about their sexual history and STI risk. Be brave, ask your doctor to test you for STIs and hepatitis B if you think you are at risk.

Get immunized against hepatitis B. Not sure if you’ve been immunized during childhood? Tell your healthcare provider and get tested and immunized. Even if you were vaccinated in the past, getting a second vaccine series won’t harm you. If your partner has hepatitis B, getting vaccinated is critical to protect your health. Get tested first. Practice safe sex until you have received all three shots. About one to two months after your third shot, get tested for the hepatitis B surface antibody (called titers). If you have at least 10 mIU/mL of surface antibodies, you are permanently protected against this serious liver disease.
Infected? In Love? Disclose. When you disclose your hepatitis B status before sex – even if it’s safe sex with a condom – you don’t jeopardize your partner’s health or his/her trust in you. Talking about hepatitis B helps reduce the stigma surrounding this infection and may prompt the person to get vaccinated. How do you tell a potential partner that you have hepatitis B? Calmly and carefully. Do some research so you have a thorough understanding about hepatitis B, which will make it easier for you to calmly explain it. The more you know, the less you fear, and the more comfortable you will be in dispelling their fears and conveying a sense of truth and integrity.
Insist on sterile medical and tattoo equipment. Hepatitis B can live for several days on hard surfaces, including improperly-sterilized and re-used syringes and other medical devices. Whether you’re going for a tattoo or to a dentist or doctor’s office, it is your right to insist that all equipment is brand new (ask to see it removed from protective packaging) and properly sterilized. Visit a licensed, professional tattoo parlor and make sure all tattoo equipment has been sterilized and that needles come out of new packages.

Infected and pregnant? Protect your baby from hepatitis B.
- Make sure your newborn gets the hepatitis B vaccine within 12 hours of birth. Nearly all hepatitis B-infected women will pass the infection onto their children during delivery, but you can stop that infection cycle. In about 90 percent of cases, immediate immunization will prevent infection. In some countries, it may be difficult to get just the single hepatitis B vaccine dose, but if you are able to immunize your baby at birth, you will have protected your child against a potentially dangerous liver disease. If you live in an area where HBIG (hepatitis B antibodies) is available, make sure your newborn is also given a dose of HBIG at birth, this adds another layer of protection against infection.
- Get your viral load (HBV DNA) tested early in your pregnancy. Some women with high viral loads (exceeding 200,000 IU/mL or 1 million copies/mL) are at high risk of infecting their newborns, even if the baby receives the first vaccine dose within 12 hours of birth. Ask your doctor to test your viral load, if it’s high, medical guidelines recommend treatment with the antiviral tenofovir during the last three months of your pregnancy to lower your viral load. If you doctor doesn’t test your viral load, be assertive and ask for the test, especially if you are HBeAg positive.
- Breastfeeding is OK, even if you have hepatitis B. If you’re infected with hepatitis B, you can safely breastfeed your baby, as long as the baby was vaccinated against hepatitis B at birth.
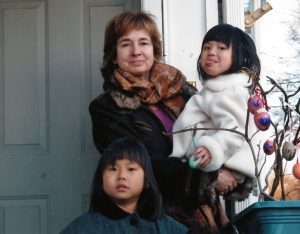
Your children infected? Don’t wait to start talking to them about hepatitis B. You need to start talking to them about germs and how to keep themselves and others safe when they’re young. (Listen to Jin’s Story #justB You about growing up with hepatitis B.) This conversation will be one of the hardest discussions you will ever have with your child, and you’ll be talking about it often in the years ahead, but you can do it! Start explaining HBV by reading the Hepatitis Victoria “Hep B Hero” book for children two to six years of age.
To hear how other mothers handled talking about hepatitis B with their children, visit our Storytelling page and click on Maureen’s Story #justB Brave and Maureen K’s Story #just B Assertive to hear how these mothers navigated issues of disclosure and stigma with their daughters. Hepatitis Victoria recently launched their “Little Hep B Hero” book, an engaging story teaching children 6-12 year olds about hepatitis B.
Talk to your children about sex and safe sex practices. It’s critical to educate young people about sexual health and STIs. If we want our sons and daughters to feel empowered to take care of their sexual health, we have to change the culture that dictates the way we talk – or don’t talk – about sex. That means removing denial, uncertainty and shame so we have better conversations about sexual health, sexual assault prevention and STIs. It’s also important to encourage our children to have frank sexual health discussions with one another.
Take care of your health, get monitored regularly: It is important to get your hepatitis B monitored regularly – at least every year and more often if you have liver damage. Women living with hepatitis B tend to have lower rates of liver damage than men because estrogen appears to help protect the liver. But even if we lead a healthy lifestyle and avoid alcohol and cigarettes, as we age our immune system weakens and our viral load (HBV DNA) can start to rise. There is no cure yet for hepatitis B, but there are effective drugs that lower viral load and reduce the risk of liver damage.

Be happy. A mother or woman who is well rested, enjoys a healthy diet, gets plenty of exercise, has good relationships with friends and family members and knows how to ask for help when she needs it, is far better equipped to be happy and be the best mother she can be. It isn’t selfish to take care of yourself. Tough times happen, and sometimes a friend or family member may need us, and we will need to be strong during difficult times. If we take care of ourselves and ask for help, in the long run happiness will prevail. For a profile in joy and courage while fighting hepatitis B in her family, watch Renseley’s Story #justB Strong.


 The
The 

 “We were left to connect the dots because the medical profession is failing to address an epidemic that kills more than 700,000 people a year,” he explained. “It’s bad enough that hepatitis B is a silent killer with few symptoms until it’s too late. It’s also ignored by Asian cultures that consider talk about deadly diseases to be taboo.”
“We were left to connect the dots because the medical profession is failing to address an epidemic that kills more than 700,000 people a year,” he explained. “It’s bad enough that hepatitis B is a silent killer with few symptoms until it’s too late. It’s also ignored by Asian cultures that consider talk about deadly diseases to be taboo.” By Christine Kukka
By Christine Kukka

 This military code historically barred people with serious medical conditions because they were considered unfit to serve, suspected to incur high healthcare costs and could pose an infection risk to fellow soldiers.
This military code historically barred people with serious medical conditions because they were considered unfit to serve, suspected to incur high healthcare costs and could pose an infection risk to fellow soldiers.
 I have found one of the best tools available are software programs that link a patient’s electronic medical record to current medical guidelines. It makes it easy for doctors to know what tests should be ordered, especially if they have never treated hepatitis B before. But they need to have the software and the desire to use it.
I have found one of the best tools available are software programs that link a patient’s electronic medical record to current medical guidelines. It makes it easy for doctors to know what tests should be ordered, especially if they have never treated hepatitis B before. But they need to have the software and the desire to use it. By Christine Kukka
By Christine Kukka But we do say that about smoking, drug addiction and alcoholism, and about some of the chronic infectious diseases that result, such as hepatitis B or C or HIV.
But we do say that about smoking, drug addiction and alcoholism, and about some of the chronic infectious diseases that result, such as hepatitis B or C or HIV.

